The first two articles in this cardiology series looked at the basics of auscultation and recognising heart murmurs and other heart sounds. This third and final article will be taking the theoretical knowledge gained previously and applying it to some case examples. We will be looking at left apical murmurs, left basilar murmurs and right apical murmurs.
| This article contains audio recordings. For the best experience, we recommend using headphones. |
Left apical murmurs
Differential diagnoses for left apical murmurs
Case example: a nine-year-old Norfolk Terrier presented with an incidental left apical systolic heart murmur at the time of annual health check and vaccination.
Mitral valve disease is the most likely differential in a dog like this (Table 1). Less likely differentials are dilated cardiomyopathy, congenital mitral dysplasia and mitral endocarditis: the latter is almost always diagnosed in dogs that are unwell. Congenital diseases are rare in older dogs like this and dilated cardiomyopathy (DCM) is all but unheard of in terriers – but anything is possible with acquired disease. Patent ductus arteriosus, ventricular septal defect and pulmonary hypertension do not typically present with mitral murmurs, so would localise differently.
| Differential diagnosis | |
|---|---|
| Most likely | Mitral valve disease |
| Possible | Dilated cardiomyopathy |
| Fairly unlikely | Mitral dysplasia |
| Least likely | Mitral endocarditis |
| Not localised to left apex | Ventricular septal defect Patent ductus arteriosus Pulmonary hypertension |
Murmur examples
Patient 1: grade III mitral murmur
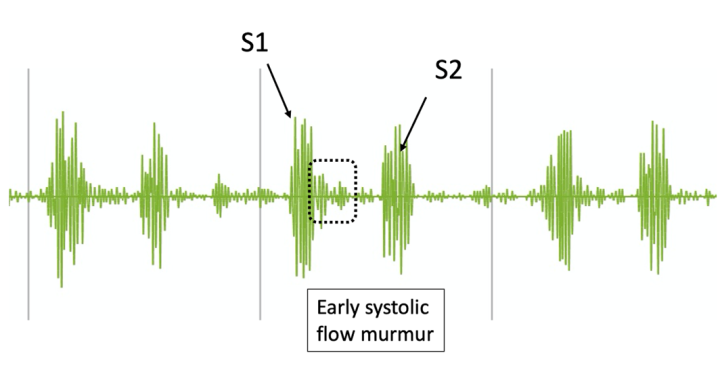
This murmur was recorded from a middle-aged terrier-breed dog with mitral valve disease which was later confirmed by echocardiography. Listen carefully to the audio of the murmur while following the phonocardiogram image (Figure 1). This is a real-life case, so the “image of the murmur” does not look like an idealised diagram (background noise, etc), but the annotations in the image should help you to identify the key components as you listen.

This was a grade III murmur. Now compare it to the following three cases of mitral valve disease in different patients.
Patient 2: grade IV mitral murmur

In this second case, we can see that the murmur amplitude on phonocardiogram is greater than the previous case, and it sounds louder than the heart sounds on the audio recording (Figure 2).
For both the grade III and grade IV murmurs we have listened to, an echocardiogram would be recommended to assess left atrial size and identify if the dog was classified as stage B1 or stage B2. It is said that 50 percent of dogs with a grade III murmur have left atrial dilation, so would be stage B2 and, therefore, would benefit from preclinical pimobendan treatment. The proportion classified as B2 with a grade IV murmur is just over 80 percent. In contrast, among dogs with a grade II murmur, only around 10 percent or below have left atrial dilation. Therefore, murmur intensity is important to stratify which dogs are most likely to benefit from investigation – this is incredibly important where cost is not unlimited, or where access to echocardiography requires a lengthy wait or referral to another practice which necessitates a long journey for the dog and owner.
Murmur intensity is important to stratify which dogs are most likely to benefit from investigation – this is incredibly important where cost is not unlimited, or where access to echocardiography requires a lengthy wait or referral
Patient 3: grade II mitral murmur
The next murmur is from a dog with a grade II mitral murmur. With these murmurs, we would tend to recommend monitoring unless the owner is very motivated to stage the disease or the dog had other concerning clinical findings (an arrhythmia or clinical signs, for example).

In this case (Figure 3), the murmur is quieter than the previous two and sounds more prominent towards the end of systole. The fact that this does not occupy all of systole again suggests the disease is at an earlier stage and the dog is less likely to be at risk of developing clinical signs or to benefit from treatment.
Patient 4: “musical” mitral murmur
Finally, we have an example of a “musical” mitral murmur. These murmurs have a resonant tone, usually because a section of the mitral valve is vibrating at a particular frequency. These murmurs are very difficult to accurately grade – the resonant tone makes the murmur radiate throughout the thorax and sound louder than it would normally do for the stage of disease.

As you can see from the phonocardiogram (Figure 4), the resonant tone of the murmur looks very different to the previous murmurs we have seen (or heard!). In this case, echocardiography showed a normal left atrial size; it is often the case that musical murmurs represent early mitral valve disease and once the musical tone disappears and the murmur sounds more coarse, the disease has progressed. This phenomenon shows how the rule that louder murmur grades mean worse disease severity cannot be applied universally – as is so often the way with biology, there are cases where the general rules do not apply.
Left basilar murmurs
Differential diagnoses for left basilar murmurs
Case example: a one-year-old French Bulldog presented with an incidental left basilar systolic heart murmur at the time of planned neutering. No diastolic component is present on careful auscultation.
Pulmonic stenosis is the most likely differential in this patient (Table 2). Aortic stenosis is possible and would localise here, but is less common in the breed than pulmonic stenosis. Since we have not specified a grade to this murmur, we could be dealing with a flow murmur if it is reasonably quiet (grade I to II, or perhaps a grade III). Aortic endocarditis is possible, but again is very rare in animals that are apparently well.
| Differential diagnosis | |
|---|---|
| Most likely | Pulmonic stenosis |
| Possible | Aortic stenosis |
| Possible | Flow murmur |
| Least likely | Aortic endocarditis |
| Not localised to left base | Ventricular septal defect Mitral valve disease Pulmonary hypertension |
In addition to the differentials listed above, murmurs caused by a patent ductus arteriosus (PDA) also localise to the left base, but are higher than aortic or pulmonic murmurs (think of the anatomy – where is a PDA compared to the semilunar valves?) and tend to be best heard behind the triceps muscle on the left. Most dogs with a PDA have a palpable thrill, so always make sure to palpate puppies thoroughly behind the triceps in order to effectively screen for a PDA, even in one of our most wriggly patients!
Murmur examples
Patient 1: holosystolic pulmonic stenosis murmur

This first case is recorded from a young Labrador with severe pulmonic stenosis (Figure 5). The murmur is a grade IV and occupies all of systole. In fact, it obscures both heart sounds, which sometimes makes people find the auscultation difficult to localise. If a murmur is diastolic, it tends to have a decrescendo profile, so the murmur intensity reduces rapidly over the first half of diastole – this means that S1 at least would be very clear. If you find a murmur that is consistent in intensity and you cannot hear the heart sounds, it must be occurring during systole.
If a murmur is diastolic, it tends to have a decrescendo profile, so the murmur intensity reduces rapidly over the first half of diastole – this means that S1 at least would be very clear. If you find a murmur that is consistent in intensity and you cannot hear the heart sounds, it must be occurring during systole
Pulmonic murmurs and aortic murmurs are indistinguishable using auscultation alone; however, aortic murmurs may be easily audible at the right base as well as the left, owing to the anatomic path of the aorta as it curves to the right and craniodorsally. If you hear a murmur at both the left and right base, and even at the thoracic inlet, then it is probably aortic in origin.
Patient 2: aortic stenosis murmur with “crescendo-decrescendo” profile

Let’s look at a murmur from a dog with severe aortic stenosis (Figure 6). The murmur is louder than both heart sounds and has a clear crescendo-decrescendo profile, meaning that it increases in intensity over the first half of systole, then reduces in intensity for the second half. This is very different to a mitral valve murmur, where the intensity is the same throughout systole, referred to as a “band profile” (Figure 7).

Patient 3: aortic stenosis murmur with a band profile
Now let’s look at an aortic stenosis murmur with a band profile, for comparison (Figure 8).

The terms “holosystolic” and “pansystolic” are often used interchangeably. Some people use the term holosystolic to mean that the murmur is audible throughout systole but does not obscure the heart sounds, and pansystolic to refer to murmurs which obscure the heart sounds. This differentiation is not one on which there is consensus in the veterinary world.
Patient 4: aortic stenosis with “to-and-fro” murmur
In some dogs with aortic stenosis, we can identify both stenosis and regurgitation because of a damaged or abnormal valve. This may be audible as a “to-and-fro” murmur – so a systolic murmur caused by stenosis and an early diastolic murmur caused by regurgitation (Figure 9).

Patient 5: endocarditis with diastolic murmur
In contrast to systolic murmurs, a diastolic murmur is often very difficult to identify – even for experienced cardiologists. We are so used to hearing systolic murmurs that, at first, we may not pick up that it is a diastolic murmur without carefully visualising the sound and timing.

The most common cause of a diastolic murmur in isolation for dogs is aortic endocarditis (Figure 10). Degenerative aortic valve disease is possible but is often trivial. This is not the case in horses, where degenerative aortic valve disease in middle- to old-age is a common and clinically important problem.
Patient 6: patent ductus arteriosus
Dogs with a PDA have a systolic and diastolic component in most cases, but it sounds very different to the “to-and-fro” murmurs that we heard earlier. Instead of two distinct murmurs with a different character, the PDA sounds like a continuous flow which peaks in intensity at mid-systole, timed with the peripheral pulse on physical examination (Figure 11).

Patients 7 and 8: flow murmurs
Finally, as we know, flow murmurs can also localise to the left base. The next two murmurs were both associated with physiologic flow in young dogs with a low-grade murmur at the left base (Figures 12 and 13). Note that the murmurs are quieter than the heart sounds and do not occupy all of systole – if you listen carefully, you can hear a short pause in the noise between the murmur and S2.

Right apical murmurs
Differential diagnoses for right apical murmurs
Case example: a 12-year-old West Highland White Terrier presented with exercise intolerance, syncope and a grade IV right apical systolic heart murmur.
| Differential diagnosis | |
|---|---|
| Most likely | Tricuspid regurgitation associated with pulmonary hypertension |
| Possible | Tricuspid regurgitation associated with tricuspid dysplasia |
| Possible | Ventricular septal defect |
| Least likely | Tricuspid endocarditis |
| Not localised to right apex | Pulmonic stenosis Aortic endocarditis Mitral valve disease |
Tricuspid regurgitation associated with pulmonary hypertension is most likely (Table 3), in part because of the murmur grade (it is difficult for tricuspid regurgitation to exceed a grade III with normal pulmonary arterial pressure), but also because of the history and signalment. West Highland White Terriers are commonly affected by pulmonary interstitial fibrosis, which is a common cause of pulmonary hypertension in older dogs. A congenital valve dysplasia is possible generally but would be very rare in this breed, and a ventricular septal defect again is possible but rare in this breed and dogs of this age. Tricuspid endocarditis would localise here but is incredibly rare (dogs tend to have the mitral and aortic valves affected only, and the right heart remains unaffected in dogs and cats – different to farm species) and the other listed differentials would localise on the left.
West Highland White Terriers are commonly affected by pulmonary interstitial fibrosis, which is a common cause of pulmonary hypertension in older dogs
Murmur example

The murmur represented in Figure 14 is from a dog with a ventricular septal defect (VSD) which was causing not only systolic flow from the left heart to the right heart (hence a right-sided murmur), but a little aortic insufficiency. This combination is not uncommon as the VSD is often positioned below the aorta, so the root of the valve falls a little to one side and the valve leaflets do not close normally in diastole. It is not usual to hear both flows, but here it is possible and serves to illustrate what is happening because of the anatomic location of the VSD in most dogs (peri-membranous; sub-aortic to sub-tricuspid).
In summary
My top tips are to keep on listening to your patients in a structured way, and try to discuss what you hear with colleagues in order to validate your findings, or provide another perspective
Auscultation is difficult, with a steep learning curve. Despite data suggesting that many recent graduates’ skills plateau soon after graduation, listening to a wide range of heart murmurs should be helpful to increase people’s confidence with hearing new things. Integrating history, signalment and auscultation findings is a valuable way to consider whether a dog requires further investigation of cardiovascular disease or not. My top tips are to keep on listening to your patients in a structured way, and try to discuss what you hear with colleagues in order to validate your findings, or provide another perspective.
| The content in this article is further discussed by Kieran Borgeat in Improve International’s Small Animal Cardiology Online Learning GPCert/PgC programme, of which Kieran is the course director. For more information, please visit the Improve International website. |









