You need to register to access this content. Registration is free and can be done below. Alternatively, you can log in or join our membership for unlimited CPD content.
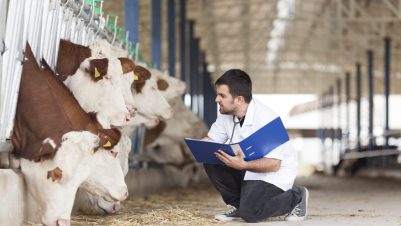
Veterinary surgeons and zoonotic diseases
The need to know more about transmission from animals to humans and the whole area of what to do about it is set for an explosion of awareness