Udder cleft dermatitis (UCD) is a common skin condition of the udder in dairy cows. The condition is characterised by an ulcerative, exudative, malodorous dermatitis, with lesions found on the anterior junction of the udder and abdomen, or between the udder halves (Figure 1).
Clinical signs of udder cleft dermatitis

UCD lesions are often overlooked due to their anatomical location, with cows rarely showing signs of systemic disease. Affected individuals may not be identified until the characteristic pungent odour develops, when lesions have generally progressed from initial skin irritation to ulceration and necrosis.
Severe lesions can have significant sequelae, including mastitis, embolic pneumonia and haemorrhage due to erosion of subcutaneous blood vessels. Millar et al. (2017)describe deaths following embolic pulmonary spread of bacteria from UCD lesions.
While it has not been assessed, it is expected that UCD has an impact on herd health production.
Aetiology, prevalence and epidemiology
The aetiology of UCD is not yet fully understood, despite the condition being first reported in the UK over 20 years ago (Beattie and Taylor, 2000). Previously, it was associated with mites (Allenstein, 1991), treponemes (Evans et al., 2010) and primary bacterial colonisation (Sorge et al., 2019).
While UCD is sometimes referred to as “udder digi”, recent studies have found no link with bovine digital dermatitis. The bacteria commonly isolated from UCD lesions are the anaerobes Truperella pyogenes and Bacteroides pyogenes, rather than the treponemes associated with digital dermatitis (van Engelen et al., 2021).
Udder conformation and parity are the most significant cow-level risk factors for UCD lesions, specifically animals with a deep udder and weak fore-udder attachment
The anterior junction of the udder and the udder cleft are prone to abrasion and ulceration. Opportunistic bacterial infection following abrasion in this anaerobic environment is the most likely aetiology of UCD lesions (Gratwick, 2025).
Udder conformation and parity are the most significant cow-level risk factors for UCD lesions, specifically animals with a deep udder and weak fore-udder attachment (Hansen and Nissen, 2010). Greater milk production and increased parity have been linked to an increased risk, likely due to the impact of these factors on udder conformation during lactation (Vermeersch et al., 2025). The understanding of herd-level risk factors is limited.
UCD scoring
Herd-level scoring can easily be done in the milking parlour, with the aid of an inspection mirror or “selfie-stick” mirror with a light source to inspect the udder cleft of each cow – as seen in Figure 2 and Figure 3 (NoBACZ Healthcare, 2025).
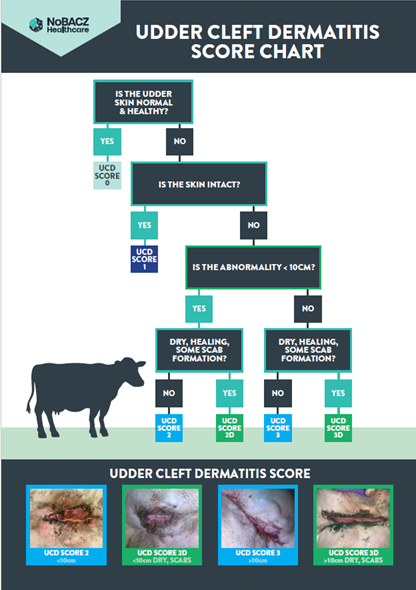
Several schemes exist for scoring UCD with lesions categorised by size and characteristics, including a scoring system created in 2024 by a UK-based UCD steering group (Girvan, 2024).


Management, treatment and prevention
Published information on UCD treatment is limited, with no accepted “gold standard” and no proven effective treatment (Vermeersch et al., 2025). This has led to the use of a variety of unproven products, potentially resulting in ineffective treatments or untreated cases (van Werven et al., 2018).
Treatment of severe UCD lesions is challenging, requiring repeated applications of a product for a prolonged period. The mean duration for a case of UCD is eight weeks for mild lesions, and between 16 and 21 weeks for severe lesions (Bouma et al., 2016; Ekman et al., 2021). Studies show mild lesions have a higher recovery rate than severe lesions, but if lesions are present for 12 weeks or longer, the recovery rate is markedly reduced (Bouma et al., 2016). This highlights the importance of regular monitoring and treatment of cows with UCD lesions.
Published information on UCD treatment is limited, with no accepted “gold standard” and no proven effective treatment
Maintaining the cleanliness of the wound, preventing infection and promoting skin healing are beneficial when managing UCD. One study found a high improvement rate in cows with severe lesions that were cleaned but had no additional treatment, compared with untreated cows (Ekman et al., 2021).
Anecdotally, lesions may improve following use of off-label medications such as antibiotic preparations, creams and salicylic acid. However, statutory withdrawal periods must be applied and communicated to the farmer, due to the risk of medicine residues in the milk of animals treated off-label (Veterinary Medicines Directorate, 2025).
Whichever product is used, the practicality and ease of applying it frequently and for a prolonged period is the limiting factor.
Culling animals with recurring lesions at the end of their lactation period and selectively breeding for favourable udder traits are considered the most effective prevention strategies. One Midlands-based dairy herd with a previous high incidence of UCD focused on selecting bulls for the fore-udder attachment and udder depth. After several years, the prevalence of UCD within the herd was 1.3 percent (Gratwick, 2025).
New approaches to UCD scoring and management
The existence of various classification systems for UCD means that establishing an accepted treatment protocol is challenging (Vermeersch et al., 2025). In 2024, a new, simplified scoring system was devised by the UCD steering group to give a clear case definition of the condition and allow more consistent monitoring, reporting and management of UCD on-farm (Figure 4) (Girvan, 2024).
An inspection stick mirror was used on several Midlands-based dairy farms to examine the anterior udder and udder cleft. UCD lesions were identified and scored using the simplified scoring system, and a zinc-based hydrophobic gel barrier product was applied with reportedly good results.
The NoBACZ zinc gel barrier product (NZGB) combines a natural bioresin complexed with zinc salts, and forms a hydrophobic, non-colonisable, physical barrier over the site where it is applied. While the barrier formed is immediately hydrophobic, the product will not seal the application site until any exudate or discharge is resolved, avoiding the risk of trapping contaminated exudate at the wound interface. The product lasts for one to three days, then naturally biodegrades and flakes off. It is a food-grade product, meaning there is no withdrawal period for milk or meat entering the food chain (Charles and Page, 2024).
Combining regular UCD scoring with mobility scoring helped identify lesions earlier, which increased the chance of recovery when treating mild compared to severe cases
Users of NZGB products advocate daily applications for three to five days, followed by bi-weekly or weekly repeats. A paper towel can be used to gently remove dirt and exudate, without removing scabs on healing lesions, and product can then be applied as in Figure 5.
Application of NoBACZ’s gel barrier products in the parlour is tolerated well (Figure 6). Gratwick (2025) reports that one farm found 77 percent of lesions healed within four to nine weeks. The remaining 23 percent of lesions were showing signs of re-epithelialisation by week nine.
A Midlands-based dairy farmer who had experienced limited success with antibiotic and non-antibiotic aerosols found that the NoBACZ gel barrier products quickly resolved the malodorous smell and exudate; with regular application over several weeks, the UCD lesions healed well (NoBACZ Healthcare, 2025).
Incorporating this technique into a monitoring programme enabled the farm to identify early cases of UCD and implement treatment protocols much earlier in the development of the lesions. Combining regular UCD scoring with mobility scoring helped identify lesions earlier, which increased the chance of recovery when treating mild compared to severe cases.




Conclusion
Identifying UCD lesions promptly through regular screening in the parlour has been shown to enable earlier detection and prompt treatment of lesions, which is associated with a higher recovery rate. Gel-barrier technology products may be a useful tool in managing UCD lesions.








