Interventional radiology (IR) involves the use of real-time imaging modalities, such as fluoroscopy, bronchoscopy and cystoscopy, to undertake minimally invasive procedures (McLauchlan, 2020). It is a recently emerged area of veterinary medicine and has gained increasing interest over the past few years. IR has many existing applications and shows promise for future options for veterinary patients. This article will discuss the benefits of IR and list some of the most common conditions we can treat (Table 1), as well as some of the equipment required to perform the procedures. Two of the procedures will then be discussed in more detail.
What are the benefits of interventional radiology?
Table 1 shows the range of diseases and conditions that can be commonly treated with IR. In some of these cases, the traditional surgical options are least favoured. Patients undergoing IR will have a small (1 to 2cm) incision, if any at all. As IR is minimally invasive, it has been associated with a reduced mortality rate compared to traditional surgical options, as well as shorter post-operative recovery times and reduced complications (McLauchlan, 2020).
| Intervention type | Disease or condition treated |
| Respiratory | Tracheal collapse Nasopharyngeal stenosis Bronchial collapse |
| Gastrointestinal | Oesophageal strictures Colonic obstructions/strictures |
| Vascular | Intrahepatic portosystemic shunts Unresectable liver tumours Prostatic neoplasia Intra-arterial chemotherapy |
| Urinary | Ectopic ureters Bladder tumours Urethral/ureteral obstruction Idiopathic renal haematuria Bladder stones |
What equipment is required for interventional radiology?
A range of specialist equipment is commonly used in IR procedures. Fluoroscopy allows real-time imaging and the unit used is called a C-arm. During procedures, it can be used alongside other modalities such as bronchoscopy or cystoscopy, and allows for radiographic views from different angles without repositioning the patient. As the C-arm is delivering X-rays, radiation precautions for the room and personal protective equipment (PPE) must be considered. You must also be compliant with the Ionising Radiations Regulations 2017 (IRR17) from the Health and Safety Executive (HSE).
Other commonly used equipment includes:
- Guidewires in a variety of sizes and types (most commonly with a hydrophilic coating)
- Introducer sheaths which are placed over a guidewire and allow placement of angiographic catheters or other devices
- Angiographic catheters which are flexible catheters that allow us to administer contrast, medications or embolic products to a targeted area. They come with a variety of different-shaped ends, but Berenstein and Cobra catheters are most commonly used with our veterinary patients
- Stents are tubular devices, which can be made of nitinol (nickel-titanium) or plastic depending on which part of the body they are used in, to relieve a luminal obstruction
- Balloon dilation catheters which enable us to dilate strictures
- Embolic products, which can be coils, microparticles in suspension or glue, can be used to occlude vessels due to their presence as well as subsequent thrombosis.
Case studies
Tracheal stenting
In the most severe cases of tracheal collapse, stenting of the trachea can be performed to reduce breathing difficulties. A nitinol mesh stent is deployed along the length of the trachea with fluoroscopic and endoscopic guidance.
Tracheal collapse is a progressive disease that is most commonly seen in Yorkshire Terriers and Pomeranians, although it can affect other small-breed dogs. The disease occurs due to progressive degeneration of the tracheal cartilage in combination with lower levels of glycosaminoglycan and a decrease of elastic fibres of the tracheal membrane, which results in dorsoventral flattening (McLauchlan, 2020).
Patients will typically present with a honking cough that is said to resemble a goose honk, produced as the trachea collapses down and the air is squeezed through it. The cough usually worsens with stress or excitement. These patients usually exhibit exercise intolerance and this will worsen in warmer weather. Environmental triggers like cigarette smoke or other inhaled irritants can also worsen their signs.
Stenting is considered a salvage procedure and should only be considered if medical management has failed or in an emergency
In the most severe cases, these patients can present dyspnoeic, cyanotic and collapsed. Stenting is considered a salvage procedure and should only be considered if medical management has failed or in an emergency. It should also be noted that patients will likely still require lifelong medical management even after stenting.
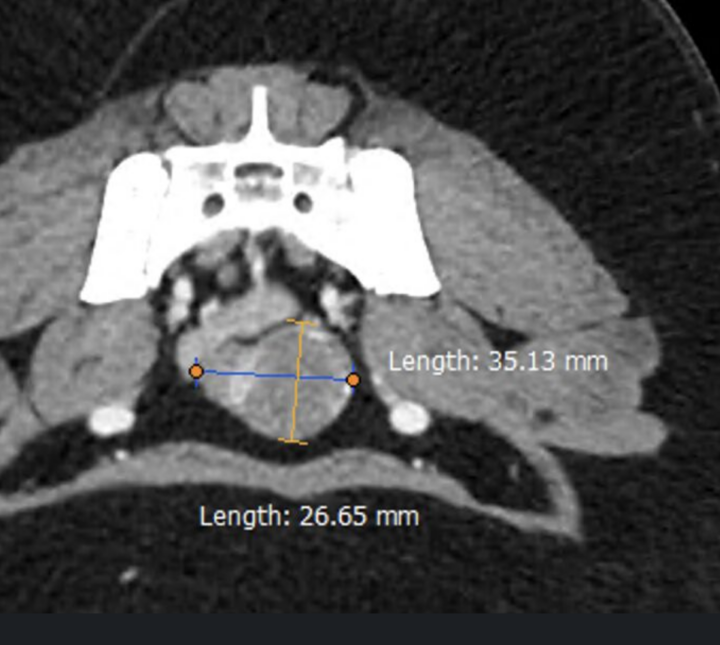
At induction, there is an endoscopic airway assessment to look at the level and area of collapse. A fluoroscopic image is then taken under positive pressure ventilation to use for taking measurements and choosing the best-sized stent for the patient. The stent is deployed with fluoroscopic assistance and the endotracheal (ET) tube is slowly removed ahead of it to prevent deployment of the stent within the ET tube. The patient is reintubated with a smaller ET tube and then a repeat endoscopic examination is performed to confirm successful placement (Figure 1).
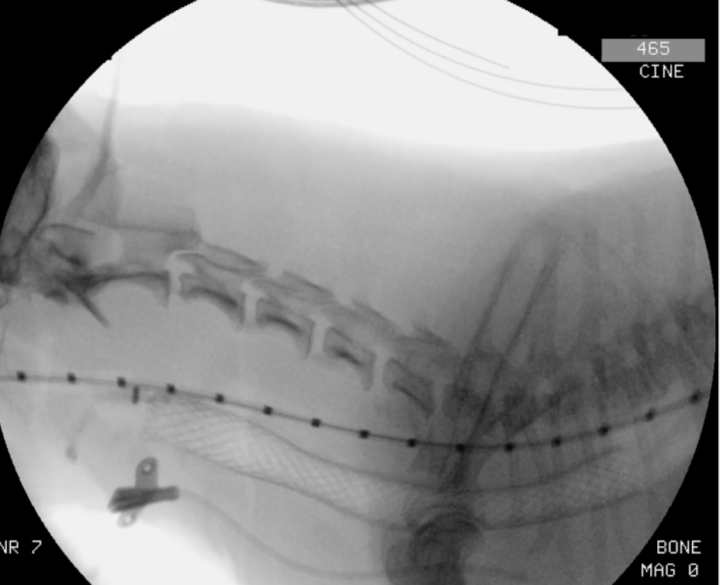
It is advisable to use total intravenous anaesthesia (TIVA) with propofol or alfaxalone for these cases to provide more consistent anaesthesia throughout, as well as to reduce environmental contamination and personnel exposure with frequent extubations and disconnections. Although many patients will have a good recovery and have fewer breathing difficulties following stenting, it is advisable to have equipment for reintubation available for the recovery period and to try to limit any stress where possible.
Prostatic embolisation
Prostatic carcinoma affects less than 1 percent of dogs and is much more common in castrated males compared to those who are entire. It is considered highly aggressive and often comes with an extremely poor prognosis (Freitag et al., 2007).
Common areas for metastases are the regional lymph nodes, spine and lungs; however, problems caused by the local disease will most commonly lead to euthanasia. Previously, the only options available to these patients and their owners were prostatectomy or chemotherapy. In 2021, William Culp reflected “poor response rates to currently available treatments for dogs with prostate neoplasia dictate the need for improved therapeutic options” (Culp et al., 2021). Embolisation of the prostatic artery is now available in a limited number of veterinary centres around the world, including in the UK.
This lack of blood supply will cause sterile necrosis of the tissue and a reduction in size which can improve clinical signs such as tenesmus and stranguria, therefore allowing the patient to be more comfortable and have better quality of life for as long as possible
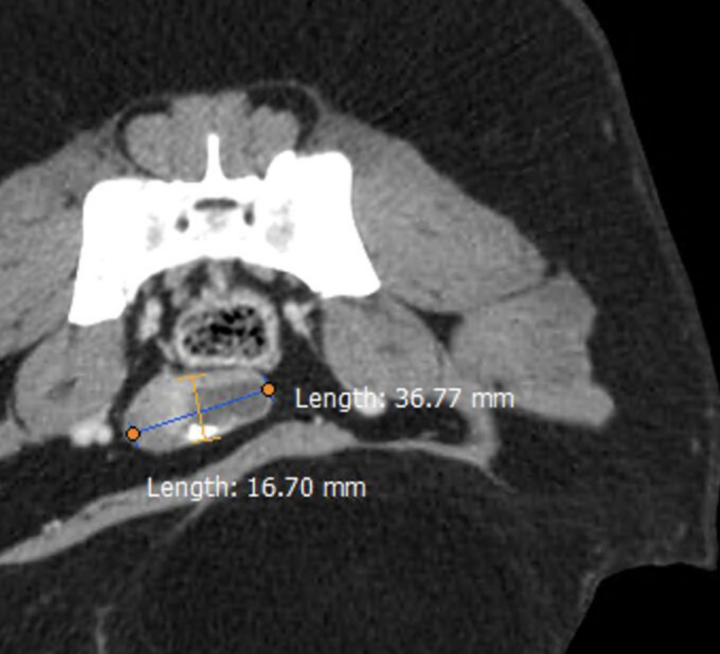
Using an approach via the carotid artery and fluoroscopic guidance, a catheter is passed down the aorta to the internal iliac artery before a microcatheter is directed into the prostatic artery, and embolic microspheres are delivered to block the blood supply to the prostate and therefore the tumour (Figure 2). Where possible, the procedure is performed bilaterally. This lack of blood supply will cause sterile necrosis of the tissue and a reduction in size which can improve clinical signs such as tenesmus and stranguria, therefore allowing the patient to be more comfortable and have better quality of life for as long as possible. The hospitalisation period can be as little as 24 hours, but a small number of patients (less than 10 percent) will develop urinary retention and require a slightly longer stay.